In 2018, seismic changes taking place in healthcare will help trigger the evolution of our nation’s healthcare system, including services available to the aging population.
Here are five key trends to watch and how they could impact the care you provide your patients.
1. Healthcare Consolidation Between Insurers and Providers
What it is: Over the past few years, the healthcare industry has seen a trend of consolidations due to declining reimbursements and increasing legislative and regulatory burdens. This promises to continue in 2018, as new mergers between insurers and care delivery operators create more integrated full-service providers. Two notable transactions leading the trend are the planned “horizontal” merger of CVS and Aetna and the acquisition of DaVita Medical Group by the Optum unit of United HealthGroup. Expect to see more insurers looking to form closer relationships with providers of lower-cost medical care.

Why it matters: Mergers and acquisitions that seek to break down traditional silos in healthcare are the next step for payers and providers.
This will benefit patients by reducing inefficiencies in care and improving care coordination. These new relationships will support the collaboration essential to the move toward value-based care, and have the potential to pass along reduced healthcare costs to consumers.
2. Addressing the Opioid Crisis
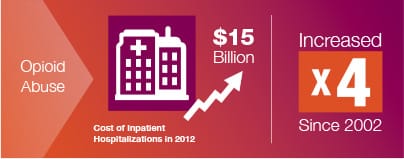
What it is: The United States is in the midst of an opioid abuse crisis. The Department of Health and Human Services reports that drug overdose deaths are the leading cause of injury death. In 2012, the cost of inpatient hospitalizations related to opioid abuse reached $15 billion, nearly quadrupling since 2002, according to Health Affairs. In 2018, intensified focus and resources will be required in order to address the crisis. Many reports suggest that the only successful path will require collaboration between government entities, payers, providers and health plans.
Why it matters: While it is essential to tackle the opioid crisis to improve the lives of up to two million Americans who are suffering from substance abuse, it is also critical to rein in the out-of-control spending caused by this epidemic. A truly collaborative approach to create solutions will establish best practices that can be applied to other patient populations, such as those with multiple chronic illnesses, to improve population health for the long term.
3. Patient Experience Continues to Rise in Importance
What it is: As healthcare furthers its transition from volume-based to value-based payment and delivery models, the measure of a positive patient experience has greater importance to healthcare providers. A number of healthcare providers, including acute hospitals, dialysis centers and home health agencies, have their patient experience scores publicly reported on Medicare.gov.
Why it matters: With consumers more involved in decisions affecting their care, a provider’s reputation as shaped by public sentiment is more important than ever. It influences not only patient engagement, but can give hospitals an advantage in establishing partnerships with payers and other providers in an increasingly collaborative healthcare environment. A positive patient experience drives reputation as well as a patient’s willingness to recommend a facility and establish loyalty. Recently, the Advisory Board Company reported that a 10 percent increase in customer loyalty could generate more than $22 million in revenue for the average hospital; therefore, healthcare providers will need to consider strategic investments to improve patient experience.
4. Expansion of Medicare Advantage
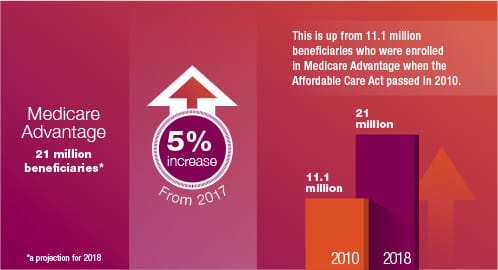
What it is: In 2018, it is projected that Medicare Advantage will cover nearly 21 million beneficiaries, which is a 5% increase from 2017. This is up from 11.1 million beneficiaries who were enrolled in Medicare Advantage when the Affordable Care Act passed in 2010. Current and projected growth has been attributed to a series of factors including the appeal of bundling doctor, hospital and drug coverage into a single plan for consumers, continued low premiums and high satisfaction rates for patients.
Why it matters: Healthcare providers and physicians need to reassess their relationships with Medicare Advantage plans. Even though Medicare Advantage reimburses at a lower rate than traditional Medicare, these plans account for the coverage of more than one third of all Medicare beneficiaries. This means that even though reimbursement levels are lower, the volume of patients could make up the difference.
5. Repeal and Replace Is Done, But Reforms Still Loom
What it is: While Congress and the President were unable to repeal and replace the Affordable Care Act (ACA) in 2017, it is likely that the government will continue to pursue health reforms in 2018. It is expected that Congress will work to reform Medicaid through block grants and reduced spending, delaying the Health Insurance Tax (HIT) and other ACA taxes, and begin to take on Medicare reform.
Why it matters: The sustained focus on Medicare and Medicaid reforms continues to provide an environment of reimbursement uncertainty for providers across the care spectrum. This environment challenges providers to innovate and create efficiencies in care delivery and will require new partnerships to ensure the delivery of optimal patient care.
How Kindred Can Help
Kindred has transformed its capabilities to meet the health and wellness needs of Americans from hospital to home, including the testing of new payment and delivery models. Our goal in transforming operations is to better deliver care and services to patients where and when they need them most, and to offer payers and other healthcare partners innovative solutions when partnered with us.
In addition to offering patient-centered post-acute services through direct operations and strategic partnerships, we are strengthening our ability to effectively managed care nationwide through our collaborations with premier hospitals and health systems and continuous innovations.
Though Kindred is best known as a provider of healthcare services, we are often asked by our patients and families for information or assistance on the broader range of challenges they face. Because of this consumer demand, Kindred established 1-866-KINDRED, staffed 24/7 by Registered Nurses who can help identify the best and most convenient care options to meet a patient’s needs – even if it’s not with Kindred.
Additionally, our AfterCare Program offers ongoing personal, consistent and compassionate communication with patients after they are discharged to the home from any line of Kindred services. This series of phone calls allows a Registered Nurse to assess their progress, thereby preventing patient decline and reducing rehospitalizations.
Kindred’s experience and lessons learned are important in helping shape new health policies as Congress and the Administration seek to establish value-based healthcare payment and delivery reforms. It also helps keep us agile so we may continue to serve our patients against the backdrop of a changing industry landscape.
For additional information regarding Kindred services please reach out to your local Kindred representative, visit us at www.Kindred.com or call us at 1-866-KINDRED.