Executive Summary
- Patients with chronic conditions avoided or delayed care during the pandemic and are now experiencing more advanced and complicated illnesses.
- Emergency departments and ICUs face staffing shortages, slowing patient throughput and exacerbating burnout.
- Medically complex patients who need continued acute care can be discharged to long-term acute care hospitals to improve patient outcomes and relieve hospital capacity burdens.
Impact of Care Avoidance During the Pandemic
Throughout the pandemic, many Americans avoided seeking medical attention out of fear of contracting the COVID-19 virus. This was especially true among those with chronic conditions.
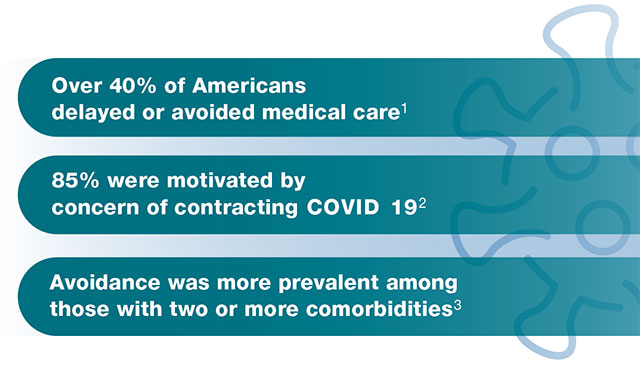
While the long-term impact of this behavior change is not yet fully known, patients and hospitals are already facing some of the consequences. Patients with underlying conditions such as obesity and diabetes are already at greater risk of developing more serious illnesses.4 Without proper management of such comorbidities, these hospitalized patients have become even more medically complex and now require an even greater intensity of care.
“Too many people are avoiding care because they’re worried about COVID-19 in hospitals and doctors’ offices. It’s not surprising, but as a physician, it is very concerning. It shouldn’t be this way,” says Cleveland Clinic CEO and President Tom Mihaljevic, MD5
Across the nation, emergency departments and ICUs are now facing an influx of patients whose conditions are more advanced and complicated as a result of delays in care. Without sufficient resources, many patients face long wait times in the ER, impacting patient outcomes and experience.
LTACHs Can Relieve Resource Constraints at the Hospital
One approach to managing patient flow and outcomes is to discharge medically complex patients who require continued acute care to a long-term acute care hospital (LTACH).
When the appropriate patients are discharged from the ICU to an LTACH, the benefits are numerous:
- Medically complex patients receive the level of care they need to fully recover
- Hospitals increase throughput
- Patients in the ER receive timely care and have a more positive experience
- Hospital staff experience less burnout
Clinical Capabilities of LTACHs That Aid in Complex Care Recovery
Physicians with sub-specialties in areas such as pulmonology and infectious disease lead interdisciplinary teams of nurses, dietitians, rehabilitation specialists, and others to provide customized care plans. Respiratory therapists also provide 24/7 coverage and specialize in liberating patients on prolonged mechanical ventilation.
Specialized Staff
LTACHs utilize the services of physicians and ICU/CCU-level nurses who are experts in treating patients with complex conditions.
In fact, patients at an LTACH are characterized as having:
- An average of six comorbidities6
- An “extreme” illness 55% of the time7
- An average case mix index of 5.19 at discharge from an STACH8
Hospital Setting
Licensed as acute care hospitals, LTACHs are equipped with on-site laboratories, telemetry, radiology, pharmacies and dialysis. With these services in house, they are able to reduce the risk of exposure to disease and of setbacks due to patient transfer.
Additionally, LTACHs feature negative pressure isolation rooms that reduce the spread of highly contagious airborne viruses and bacteria. Infection control standards, overseen by a specialized Infection Prevention Nurse, also comply with the requirements of the Centers for Medicare and Medicaid Services (CMS) for general acute care hospital licensing.
How Kindred Hospitals Can Help
Kindred Hospitals has provided quality care for 30 years, and continue to introduce initiatives that improve care, such as:
- Pursuit of disease-specific certifications from The Joint Commission in Sepsis and in Respiratory Failure in all hospitals
- Early mobility programs that incorporate mobilization as early as is safe, even for patients on ventilators, allowing for a quicker, more complete recovery
- Their proprietary AfterCare program, in which specially trained RNs follow up with patients post-discharge to discuss durable medical equipment and medication needs and education, primary care provider appointments, and any additional post-discharge services needed
If you have a medically complex patient in need of acute care after a hospital stay, call a Kindred Clinical Liaison for a patient assessment. Our Clinical Liaison team will help you determine whether an LTACH stay is appropriate for your patient. If you are unsure of who your Kindred representative is, please feel free to contact us via recoveratkindred.com and speak with a Registered Nurse who can assist.
References
- https://www.cdc.gov/mmwr/volumes/69/wr/mm6936a4.htm
- https://consultqd.clevelandclinic.org/americans-avoid-seeking-medical-care-during-pandemic-survey-shows/
- https://www.cdc.gov/mmwr/volumes/69/wr/mm6936a4.htm
- https://www.yalemedicine.org/conditions/ards
- https://consultqd.clevelandclinic.org/americans-avoid-seeking-medical-care-during-pandemic-survey-shows/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3094575/
- https://www.aha.org/system/files/media/file/2019/04/fact-sheet-ltch-0319.pdf
- Calculations from MedPar 2020 data